
New state reports detail drivers behind rising health care costs in New Jersey
TRENTON, N.J. — Rising health care costs in New Jersey are being driven largely by higher prices across the system rather than increased use of services, according to a series of new reports released Friday by the Office of Health Care Affordability and Transparency in the state Department of Health.
The five reports provide an in-depth look at health care spending trends, cost drivers and the overall health care landscape in New Jersey, offering what officials described as unprecedented transparency into a sector that accounts for nearly 11% of the state’s gross domestic product.
“We know that health care costs strain New Jersey families. Addressing affordability requires each part of the health care system to examine its role and take meaningful action to make health care affordable in our state,” said Acting Health Commissioner Jeff Brown. “These reports are essential tools to inform that work, providing critical clarity to help us rein in health care costs.”
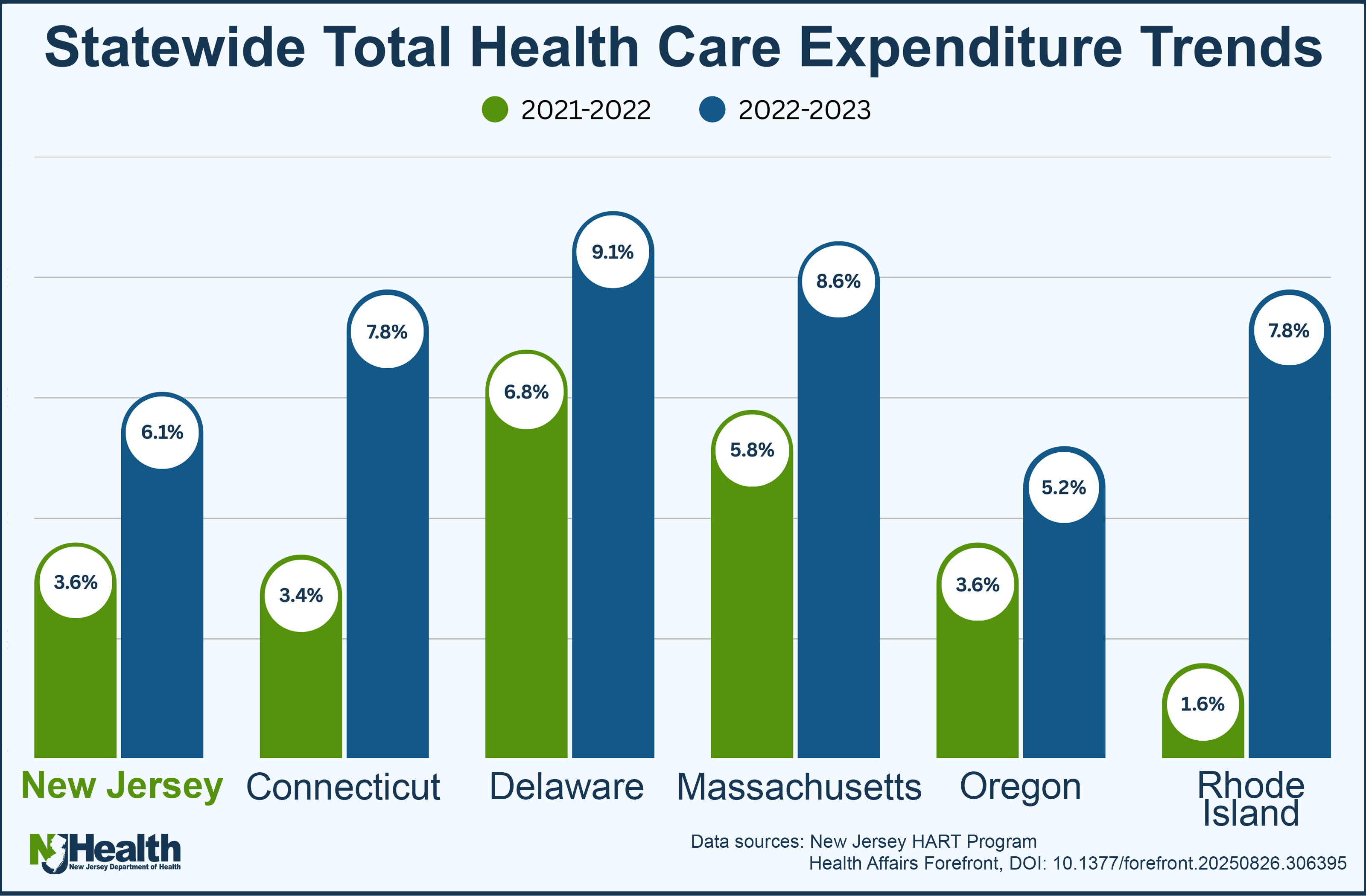
Two of the reports analyze health care spending under the Health Care Affordability, Responsibility, and Transparency Program’s cost growth benchmark, examining a transition year from 2021 to 2022 and the first performance year from 2022 to 2023. Together, they show that costs increased across nearly all insurance markets, service categories, insurers and providers.
State officials reported that average per-person health care spending rose 3.6% from 2021 to 2022, increasing from $10,292 to $10,663 annually. Total statewide health care spending rose by $3.95 billion, or 5.1%, during that period. From 2022 to 2023, per-person spending increased 6.1% to $11,319, while total spending rose 9.2%, or $7.42 billion.
The performance year marked the first time insurers and providers were measured against the state’s 3.5% cost growth benchmark, established under a voluntary compact launched by Gov. Phil Murphy to slow health care spending growth between 2022 and 2027.
“The reports provide transparency into New Jersey health care unlike ever before,” said Jim Lloyd, executive director of the Office of Health Care Affordability and Transparency. “The results presented in these reports can inform data-driven conversations to address this systemic problem, and everyone can play a role to enhance health care affordability.”
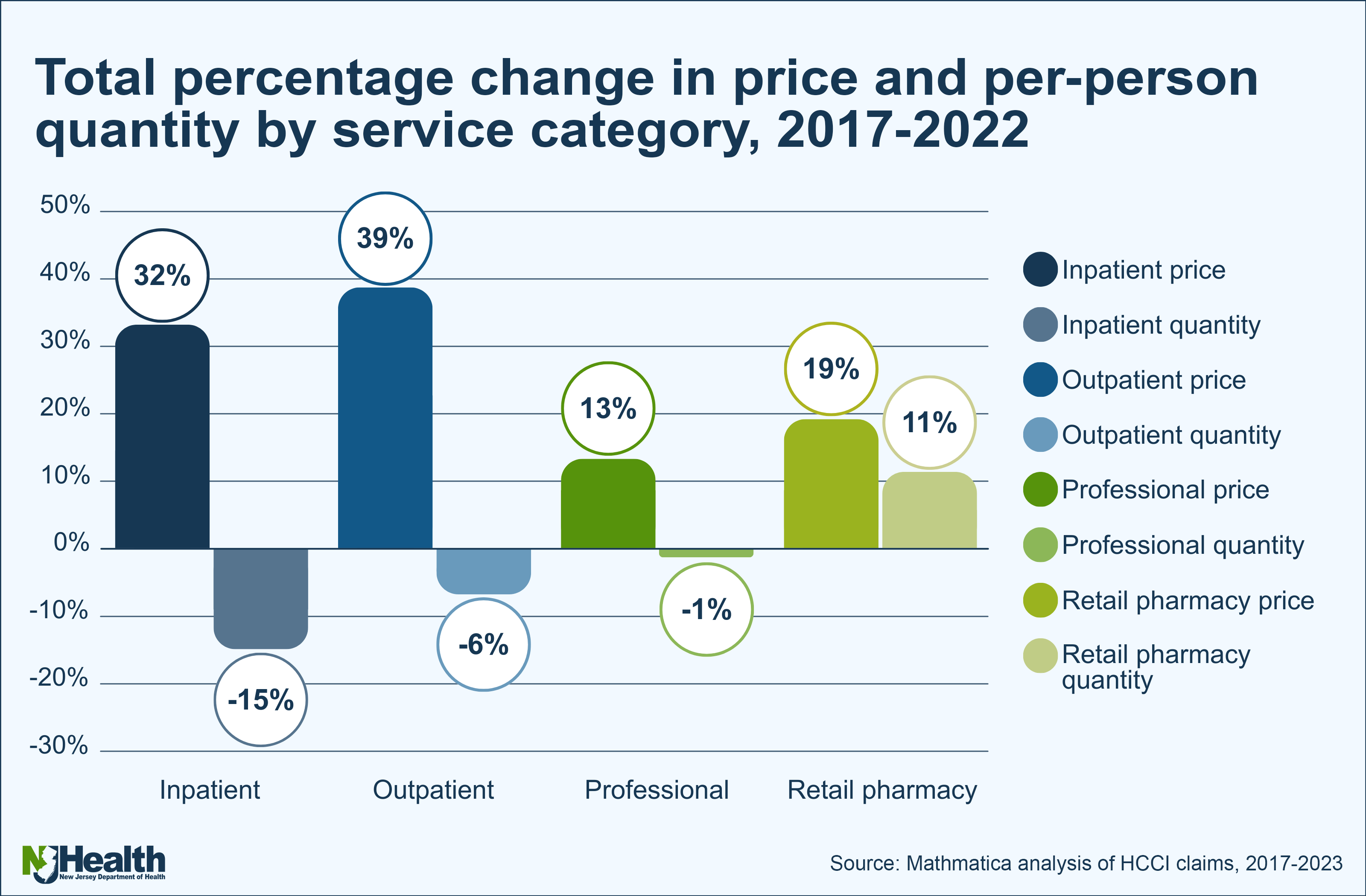
Two additional reports focused on what is driving cost increases. One analysis of commercial insurance claims from 2017 to 2022 found that rising prices, not higher utilization, were the primary factor behind increased spending. The report also found that New Jersey spends significantly less on primary care than the national average, with declining use of primary care services over the study period.
A separate report examining hospital labor costs found that while hospital operating margins declined from 2017 to 2023, non-labor costs grew faster than labor costs, and spending on direct patient care labor increased more slowly than other expenses.
The fifth report, The Health Care Landscape in New Jersey 2025, provides a broad snapshot of health care quality, access, affordability and workforce sustainability. While the report found that health care quality in New Jersey generally compares favorably to national averages, it also identified declines in several indicators and persistent disparities.
According to the report, non-Hispanic Black residents experienced the poorest outcomes on quality measures, while Hispanic residents fared worst on access-related measures. Geographic disparities were also identified, with lower-quality outcomes concentrated in parts of southern New Jersey.
State officials said the reports are intended to guide future policy decisions as New Jersey continues efforts to curb health care costs, reduce medical debt and expand consumer protections.
The reports are the first issued by the Office of Health Care Affordability and Transparency since it was moved into the Department of Health under an executive order signed by Murphy.





